G.E.R.D.
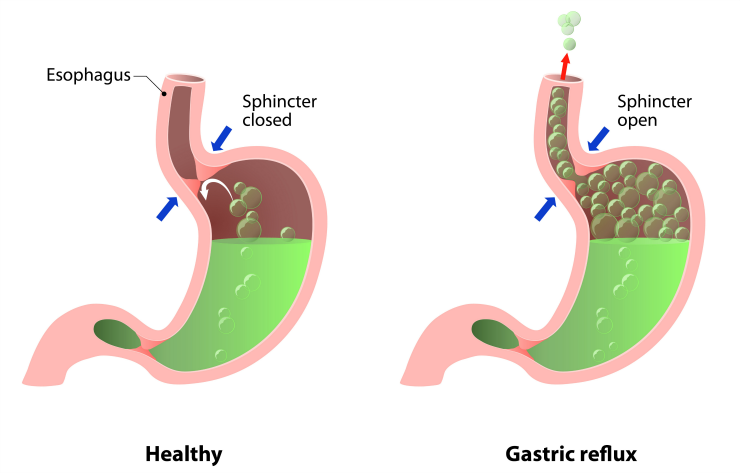
Gastroesophageal reflux disease (GERD) is a chronic digestive disease that occurs when stomach acid or, occasionally, bile flows back (refluxes) into your food pipe (esophagus). The backwash of acid irritates the lining of your esophagus and causes GERD signs and symptoms that are generally referred to as heartburn or reflux. In addition to heartburn symptoms, severe GERD can also cause problems with worsening asthma, recurrent pneumonia, or chronic laryngitis. The treatment for GERD is usually begun with lifestyle modification and diet changes. When this is insufficient, medications can be added to manage the symptoms. For some patients these treatments might not be enough and surgery may be indicated.
SYMPTOMS:
Heartburn, also known as acid indigestion, is the most common symptom of GERD and usually feels like a burning chest pain which begins behind the breastbone and moves upwards to the neck and throat. Some people experience acidic or bitter taste. Other symptoms of GERD include:
- Chest pain
- Difficulty in swallowing (dysphagia)
- Dry cough
- Hoarseness or sore throat
- Regurgitation of food or sour liquid (acid reflux)
- Sensation of a lump in your throat
DIAGNOSING GERD:
Upper endoscopy
A camera with a light is mounted on a thin, flexible tube (endoscope) which is inserted down your throat. The camera allows your physician to examine the inside of your esophagus and stomach. An endoscopy may detect inflammation of the esophagus (esophagitis) or other complications of GERD that other diagnostic tests do not. During an endoscopy, your physician may also collect a tissue sample which can be tested (biopsy) for other digestive disorders such as Barrett’s esophagus.
X-ray of your upper digestive system.
For this test, you drink a chalky liquid (barium sulfate) which coats the inside lining of your digestive tract. This allows your doctor to see your esophagus, stomach, and upper intestine and can help determine the cause of swallowing issues, unexplained vomiting, and severe indigestion. Some patients may also be asked to swallow a barium pill. This helps diagnose swallowing issues caused by a narrowing of the esophagus.
Ambulatory acid (pH) probe test
This test monitors when and how long stomach acid regurgitates into your esophagus. A monitor is inserted into your esophagus and sends the information to a small device that you wear around your waist or on a strap over your shoulder. A clip (the monitor) is placed in your esophagus during an endoscopy. The monitor is passed into your stool after about two days.
Esophageal manometry
This test measures the contraction and relaxation of your esophagus when you swallow to diagnose swallowing problems. Your nose is numbed to minimize discomfort while a tube is placed through your nose. The tube travels into your esophagus and stomach and records pressure measurements. The test also measures the coordination and force exerted by the muscles of your esophagus.
TREATMENT:
The indications for anti-reflux surgery include:
A patient who does not want to take proton pump inhibitor (PPI) medications for life
People who develop comp
lications from PPIs Patients who are allergic to PPI medications
Patients who develop resistance to PPI medications
Patients who develop comp
lications from GERD despite taking PPI medications. (i.e., bleeding, ulcers, strictures) Patients who have proximal reflux comp
lications. (i.e., asthma, hoarseness, pneumonia)
TREATMENT OPTIONS:
MAGNETIC SPHINCTER PROCEDURE
A small magnetic sphincter device is implanted by the surgeon around the outside of the lower esophageal sphincter to tighten the opening and prevent stomach acid from entering the esophagus. The device is a small implant comprised of interlinked titanium beads with magnetic cores that is placed during a minimally invasive laparoscopic procedure. Following the procedure, patients with the device may eat normally.

TIF PROCEDURE
TIF is a minimally invasive procedure to restore your esophageal valve. The surgeon uses an endoscopic device that enables him to reach the valve and stomach without the need for incisions. The procedure lengthens the esophagus, then the top of the stomach is gently folded and partially wrapped around the lower esophagus. It is held in place with fasteners made of benign material physicians have used inside the body for decades.
NISSEN 360 DEGREE FUNDOPLICATION
In this procedure, the surgeon wraps the upper part of the stomach (the gastric fundus) around the lower end of the esophagus and stitches it into place. This reinforces the closing function of the lower esophageal sphincter and helps prevent the reflux of gastric acid into the esophagus.
TOUPET 270 DEGREE PARTIAL FUNDOPLICATION
Toupet 270 degree fundoplication in which the upper part of the stomach is secured to the back of the lower esophagus at the 10:00 and 2:00 positions creating a partial wrap
REVISION ANTI-REFLUX SURGERY
A small sub-group of patients who undergo anti-reflux surgery for GERD may initially do well and then experience recurrent symptoms or complications because of a recurrent hiatal hernia or issues related to their wrap or Linx device. These patients are candidates for a laparoscopic revision procedure to address their issues.