ACHALASIA:
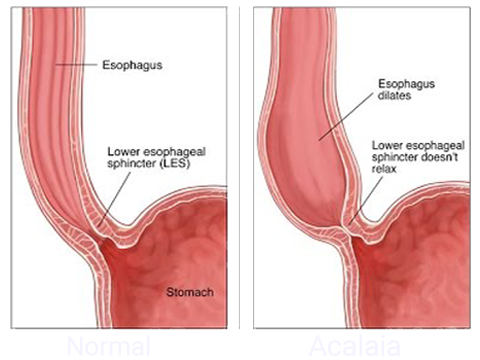
Achalasia occurs when the food tube (esophagus) loses the ability to squeeze food down, and the muscular valve between the esophagus and stomach doesn’t fully relax. The reason for these problems is damage to the nerves in the esophagus. There is no cure, but achalasia symptoms can usually be managed with minimally invasive (endoscopic) therapy or surgery.
Patients with achalasia may experience esophageal spasms or esophageal diverticuli. Esophageal spasms are irregular, uncoordinated and sometimes powerful contractions of the esophagus causing problems with food sticking or chest pain. The symptoms can happen on their own with eating or may be stimulated by heartburn. There are two main types of esophageal spasm: diffuse esophageal spasm and jackhammer esophagus.
Esophageal diverticuli are sacs or pouches which can arise in the esophageal lining between the throat and stomach. There are different types of esophageal diverticuli based on the location in the esophagus and can be treated surgically if they are associated with significant symptoms.
The use of advanced laparoscopic techniques in the management of Achalasia has dramatically improved the treatment of the condition. Traditionally, surgery involved making a large incision through the chest and patients were often in the hospital for 1-2 weeks and had significant recovery issues because of pain from the incision. Now patients can undergo laparoscopic procedures that are less invasive and allow patients to be discharged the day following surgery and are back to work within days. More importantly, more than 90 % of patients have excellent results and report no further dysphagia symptoms.
SYMPTOMS:
- Difficulty swallowing, characterized by a feeling of food caught in the throat
- Regurgitation of swallowed food and saliva
- Pain when swallowing
- Cough
- Neck pain
- Pulmonary aspiration (the entry of secretions or foreign material into the trachea and lungs)
- Aspiration pneumonia (a lung infection caused by pulmonary aspiration).
DIAGNOSING ACHALASIA:
Upper endoscopy
A camera with a light is mounted on a thin, flexible tube (endoscope) which is inserted down your throat. The camera allows your physician to examine the inside of your esophagus and stomach. An endoscopy may detect inflammation of the esophagus (esophagitis) or other complications of GERD that other diagnostic tests do not. During an endoscopy, your physician may also collect a tissue sample which can be tested (biopsy) for other digestive disorders such as Barrett’s esophagus.
Esophageal manometry
This test measures the contraction and relaxation of your esophagus when you swallow to diagnose swallowing problems. Your nose is numbed to minimize discomfort while a tube is placed through your nose. The tube travels into your esophagus and stomach and records pressure measurements. The test also measures the coordination and force exerted by the muscles of your esophagus.
X-ray of your upper digestive system.
For this test, you drink a chalky liquid (barium sulfate) which coats the inside lining of your digestive tract. This allows your doctor to see your esophagus, stomach, and upper intestine and can help determine the cause of swallowing issues, unexplained vomiting, and severe indigestion. Some patients may also be asked to swallow a barium pill. This helps diagnose swallowing issues caused by a narrowing of the esophagus.
TREATMENT:
Advanced laparoscopic and thoracoscopic techniques are used in the management of patients with esophageal motility disorders. Typically, patients with these types of disorders are older and have multiple medical conditions. In the past, many patients were not referred for surgery because of concerns that they would not survive this type of surgery. However, the use of these minimally invasive techniques has transformed our ability to address these conditions.
Achalasia is managed by performing a myotomy by cutting the lower esophageal sphincter which is causing obstruction of food as it passes from the esophagus to the stomach. This is called a Heller Myotomy.
Diverticuli of the esophagus are managed by resecting the pouches that form in the wall of the esophagus.
Jackhammer Esophagus is usually managed with medicine. On rare occasions, the entire esophagus might be removed to address this condition.